Medicare Advantage BIN-PCN-GN – What It Is and Why It Matters
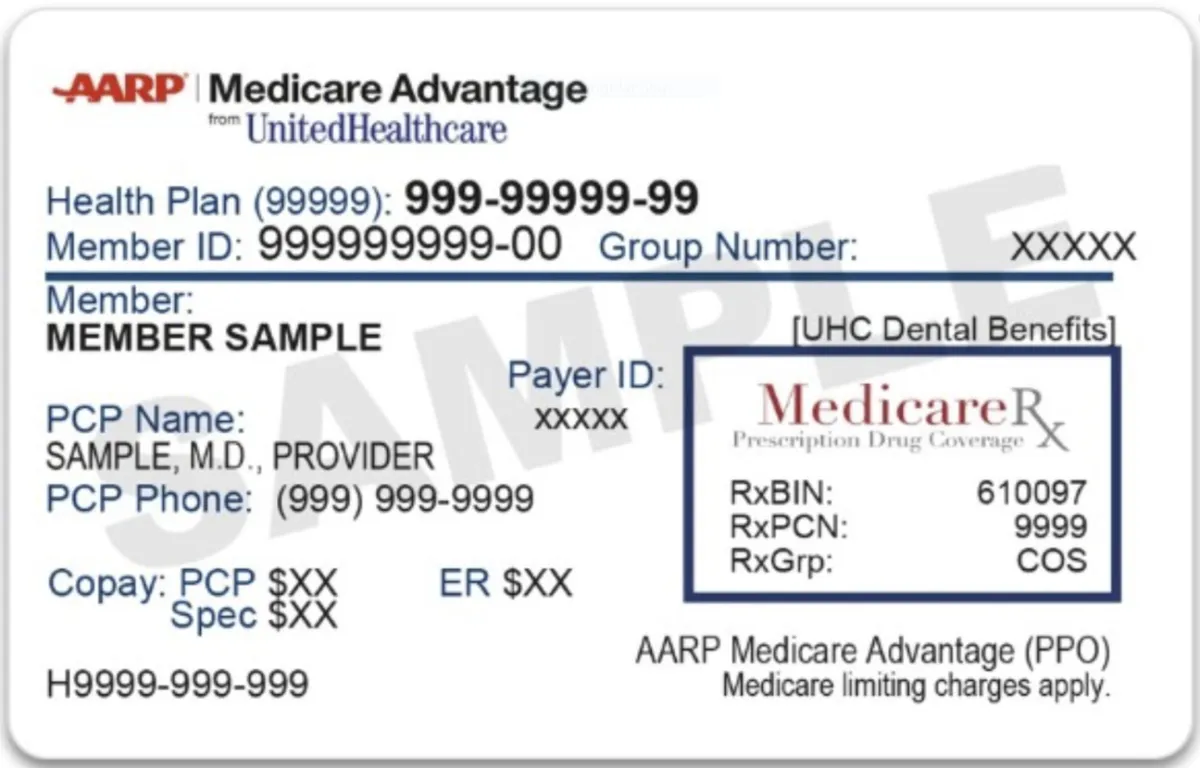
If you have a Medicare Advantage plan—especially one that includes prescription drug coverage—you’ve probably noticed some small sets of numbers and letters on your card: BIN, PCN, and GN (or sometimes GRP). These aren’t random codes. They’re important identifiers that tell your pharmacy how to process your prescriptions.
The problem? Many beneficiaries don’t know what these numbers mean, why they matter, or how errors in them can lead to delays—or even higher costs—at the pharmacy. In this guide, we’ll break down BIN, PCN, and GN in clear, simple terms so you can feel confident every time you hand over your Medicare Advantage card.
3 Key Points You Should Know Before We Dive In
BIN, PCN, and GN are routing numbers that help your pharmacy’s computer bill with the right plan for your prescriptions.
Errors in these numbers can lead to claim rejections or wrong charges.
Always check your card when you enroll or change plans—mistakes do happen.
What is BIN?
BIN stands for Bank Identification Number, but in the world of prescription drugs, it’s really a Billing Identification Number.
Purpose: It routes your pharmacy claim to the right insurance processor.
Example: Think of it like the zip code for your prescription—it gets the claim to the right “address” in the computer system.
If the BIN number is wrong or missing, your prescription can’t be billed correctly, which means delays or full out-of-pocket costs until it’s fixed.
What is PCN?
PCN means Processor Control Number.
Purpose: It’s like a sub-address that tells the processor which specific plan or program to bill within that insurance network.
Example: If the BIN gets your prescription to the right building, the PCN gets it to the right apartment inside that building.
A wrong PCN could mean your claim is billed to the wrong plan tier, giving you the wrong copay—or worse, a rejection.
What is a GN (or GRP)?
GN is short for Group Number. Sometimes you’ll see GRP instead.
Purpose: It identifies the specific group or employer plan, even within the same insurance company.
Example: It’s like naming the family that lives in that apartment—your GN tells the processor which “family” (or group) the prescription belongs to.
Why These Numbers Are on Medicare Advantage Cards
When you enroll in a Medicare Advantage plan that includes Part D prescription coverage, your insurance company sends you a card. The BIN, PCN, and GN on that card are essential for pharmacies to bill your plan’s pharmacy benefit manager (PBM) correctly.
These codes:
Speed up claim processing.
Reduce manual entry errors.
Ensure you pay the correct copay.
What Happens if They’re Wrong?
If your card has an incorrect BIN, PCN, or GN:
Pharmacy may not be able to process your claim.
You could be charged full retail price until the issue is fixed.
Your medication could be delayed if the pharmacy has to contact your plan for corrections.
This is why it’s critical to check your card when you first receive it, and every time you change plans.
How to Check and Update Your Information
Compare Your Card to Your Plan Documents: Make sure the numbers match what’s in your welcome packet.
Call Your Plan if You See Errors: Ask them to confirm and, if needed, send you a corrected card.
Bring the Updated Card to Your Pharmacy: So, they can enter the correct information in their system.
BIN, PCN, and GN in Mail-Order Pharmacies
If you use mail-order prescriptions, these numbers still matter. Mail-order pharmacies also rely on BIN/PCN/GN to process your orders correctly. If they’re wrong, you may experience:
Delays in shipping
Incorrect charges
The need to reprocess claims manually.
A Real-Life Example
Imagine Mary, a new Medicare Advantage member, getting her first prescription filled. The pharmacy’s computer rejects the claim, saying “Plan not found.” After 20 minutes on the phone, the pharmacist discovers the BIN number was entered incorrectly during enrollment. Once corrected, the claim goes through in seconds, and Mary’s $200 bill drops to her normal $10 copay.
Tips to Avoid BIN-PCN-GN Problems
Always carry your most recent Medicare Advantage card—don’t use last year’s card after a plan change.
Update your pharmacy as soon as you change plans.
Double-check your welcome letter for the right codes.
Conclusion
BIN, PCN, and GN might seem like small details on your Medicare Advantage card, but they play a big role in making sure your prescriptions are billed and covered correctly. A quick check now can save you time, money, and frustration later.
At Senior Help And You, we guide our clients through every step of Medicare enrollment—right down to the details on your ID card—so nothing slips through the cracks. Whether you’re joining a plan for the first time or making a change, we help ensure you have the right coverage and that your pharmacy experience is smooth and stress-free.
3 Takeaways
BIN, PCN, and GN are essential for correct prescription billing.
Wrong or outdated codes can cause rejections, delays, or higher costs.
Always check your new Medicare Advantage card and update your pharmacy.
Sources:
1. Medicare.gov – “Medicare Advantage Plans” (https://www.medicare.gov/medicare-advantage)
2. National Council for Prescription Drug Programs (NCPDP) – BIN and PCN Number Standards (https://www.ncpdp.org)
3. Pharmacy Times – “Understanding BIN and PCN Numbers on Insurance Cards” (https://www.pharmacytimes.com)
Author: Albert Ferrin, Senior Help and You
